Short vs. Long Antibiotic Course for Ventilator-associated Pneumonia (VAP) and Pseudomonas VAP
- Mazen Kherallah
- May 22, 2022
- 5 min read
Updated: Apr 9, 2023

Ventilator-associated pneumonia (VAP) is the most common infection among critically ill ventilated patients and it accounts for about 25% of infections in intensive care units (ICUs). It remains a major cause of morbidity and mortality in ICU. The microbiology of VAP varies between different countries and hospitals and every unit should rely on its epidemiological data and antibiograms to determine the likely cause. In a prospective observational study evaluating 158,519 patients at the University of North Carolina Hospital for 4 years, a total of 327 episodes of VAP were identified and the infecting flora included methicillin-susceptible S. aureus (MSSA; 9%), MRSA (18%), P. aeruginosa (18%), Stenotrophomonas maltophilia (7%), Acinetobacter spp (8%), and other species (9%) [1]. In a large multicenter survey of gram-negative aerobic bacteria isolated from patients in the ICU in the US, P. aeruginosa was the most commonly isolated gram-negative aerobic bacterium (23 percent) [2].
The optimal duration of antibiotic therapy for ventilator-associated pneumonia remains debated. Traditionally, VAPs have been treated with a longer duration of antibiotic therapy of at least 12-14 days. Various studies have investigated the potential of shortening the duration of antibiotic therapy in VAP to reduce patient antibiotic exposure and decrease the emergence of multi-resistant.
In a prospective double-blind clinical trial that was conducted in 51 French ICUs, a total of 401 patients diagnosed with VAP were randomized to receive either antimicrobial therapy for 8 days (197 patients) or 15 days (204 patients). Patients in the short-duration group had more mean antibiotic-free days compared to the long-duration group (13.1 vs 8.7 days, P<.001), with no significant difference in all-cause mortality (18.8% vs.17.2%) or recurrent infections (28.9% vs 26.0%). However, patients in the short-duration group with VAP caused by nonfermenting gram-negative bacilli, including Pseudomonas aeruginosa, had a higher pulmonary infection recurrence rate compared to the long-duration group (40.6% vs 25.4%) [3].
In another prospective open-label multicenter study, 225 patients with early-onset ventilator-associated pneumonia (>24 hours and <8 days) were randomized to either receive antimicrobial therapy for 8 days (116 patients) or 15 days (109 patients). Clinical cure at 21 days wasn't significantly different between the respective groups (85.3% vs. 84.4%) nor was the 21-day and 90-day mortality rates. However, similar to the study mentioned previously, the secondary infection rate was higher in the 8-day group compared to the 15-day group (35.3% vs. 19.3%, P<0.001). Of note, the study did not differentiate between fermenting and nonfermenting gram-negative bacilli [4].
In a pilot study, 30 patients diagnosed with VAP were randomized to a 7-day course of antibiotics (14 patients) versus a 10-day course (16 patients.) 14-day and 28-day mortality rates were not significantly different between the 7-day group and 10-day group (7.1 and 35.7% vs. 31.2 and 37.5%). The number of days without antibiotics was higher in the 7-day course (4.14 vs 1.75). Unlike the previous studies, the recurrence rate of infection was not significantly different between the two groups (14.3% vs 12.5%, p = 0.6). The author concluded that a 7-day antibiotic regimen was as efficient clinically and microbiologically as a 10-day antibiotic regimen with a reduction of antibiotic use. However, the larger study has never been published [5].
Furthermore, Kollef et al. investigated the outcome of a 7-day course of doripenem compared to a 10-day course of imipenem-cilastatin in a prospective double-blinded randomized trial that included 274 patients with VAP caused by Gram-negative bacteria. Clinical failure and mortality were non-significantly higher in the 7-day course of doripenem compared to the 10-day course of imipenem-cilastatin (54.4% vs 43.2% and 21.5% versus 14.8% respectively). The authors cautioned clinicians that consideration should be given to treating patients with VAP for more than seven days to optimize clinical outcomes [6].
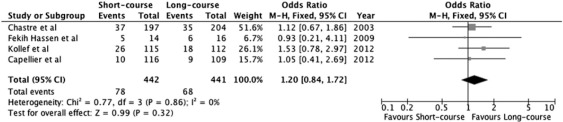
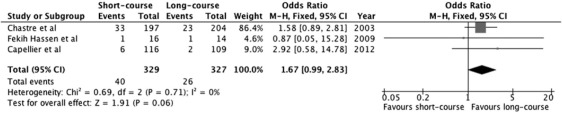
The above four trials were included in a meta-analysis that was published in 2013 and demonstrated no difference in mortality but an increase in antibiotic-free days in favor of the short-course treatment compared to a long-course treatment. There was also no difference in relapses between the compared arms but a strong trend to lower relapses in the long-course treatment was observed [7].
Based on the previous studies, it was concluded that a shorter antibiotic course has a comparable clinical efficacy for ventilator-associated pneumonia (VAP) compared to a traditional long-duration course, except for documented VAP of non-fermenting Gram-negative bacilli, including Pseudomonas aeruginosa (PA). Clinical practice adapted accordingly and reflected an understanding of the published literature by using 7-day antibiotic courses for most VAPs except for non-fermenting Gram-negative bacilli where a longer course is favored.
A recently published (May 2022) randomized open-label multicenter non-inferiority trial in France investigated the composite outcome of mortality and infection recurrence in patients with pseudomonas aeruginosa ventilator-associated infection (PA-VAP) between patients receiving an 8-day versus a 15-day antibiotic course. A total of 186 patients with PA-VAP were included in the study and the composite outcome did not differ significantly between the two groups (35.2% in the 8-day group vs. 25.5% in the 15-day group, difference of 9.7%, 90% CI: 0.0–21.2%). The percentage of recurrence of PA-VAP during the ICU stay was 9.2% in the 15-day group versus 17% in the 8-day group. Patients in the 8-day group were twice as likely to have a PA-VAP recurrence as those in the 15-day group. Despite this, the shorter therapy wasn't associated with a longer duration of mechanical ventilation or length of ICU stay. However, the study failed to recruit the required number of patients (600 patients) for 80% power. Therefore, the study lacks enough power to show a non-inferiority of the 8-day course [8].
In conclusion, the optimal duration of antibiotic therapy for pseudomonas VAP remains unclear and the decision is based on clinical judgment bearing in mind the higher rate of recurrence. In general, we rely on the patient's underlying comorbidities, the severity of illness, the susceptibility of the organism, and the response to treatment to determine the duration. Clinically we can deduce that in cases with susceptible organisms, no serious comorbidities, no bacteremia, and good initial treatment response, we can give a 7-10 day antibiotic course, otherwise, a 10-21 day course may still be warranted.
REFERENCES
1. Weber DJ, Rutala WA, Sickbert-Bennett EE, Samsa GP, Brown V, Niederman MS. Microbiology of ventilator-associated pneumonia compared with that of hospital-acquired pneumonia. Infect Control Hosp Epidemiol. 2007;28(7):825-831.doi:10.1086/518460
2. Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA. 2003;289(7):885-888. doi:10.1001/jama.289.7.885
3. Chastre J, Wolf M, Fagon JY et al (2003) Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA 290(19):2588. https://doi:10.1001/jama.290.19.2588
4. Capellier G, Mockly H, Charpentier C et al (2012) Early-onset ventilator-associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. PLoS ONE 7(8):e41290. https:// doi.org/10.1371/journal.pone.0041290
5. Fekih Hassen M, Ayed S, Ben Sik Ali H, Gharbi R, Marghli S, Elatrous S (2009) Duration of antibiotic therapy for ventilator-associated pneumonia: comparison of 7 and 10 days. A pilot study. Ann Fr Anesth Reanim 28(1):16–23. https://doi.org/10.1016/j.annfar.2008.10.021
6. Kollef, M. H., Chastre, J., Clavel, M., Restrepo, M. I., Michiels, B., Kaniga, K., Cirillo, I., Kimko, H., & Redman, R. (2012). A randomized trial of 7-day doripenem versus 10-day imipenem-cilastatin for ventilator-associated pneumonia. Critical care (London, England), 16(6), R218. https://doi.org/10.1186/cc11862
7. Dimopoulos G, Poulakou G, Pneumatikos IA, Armaganidis A, Kollef MH, Matthaiou DK. Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest. 2013;144(6):1759-1767. doi:10.1378/chest.13-0076
8. Bouglé A, Tuffet S, Federici L, et al. Comparison of 8 versus 15 days of antibiotic therapy for Pseudomonas aeruginosa ventilator-associated pneumonia in adults: a randomized, controlled, open-label trial [published online ahead of print, 2022 May 13]. Intensive Care Med. 2022;10.1007/s00134-022-06690-5. doi:10.1007/s00134-022-06690-5


留言