End-expiratory Occlusion test and the assessment of transpulmonary pressure
- Mazen Kherallah

- Sep 27, 2022
- 3 min read
Updated: Apr 9, 2023
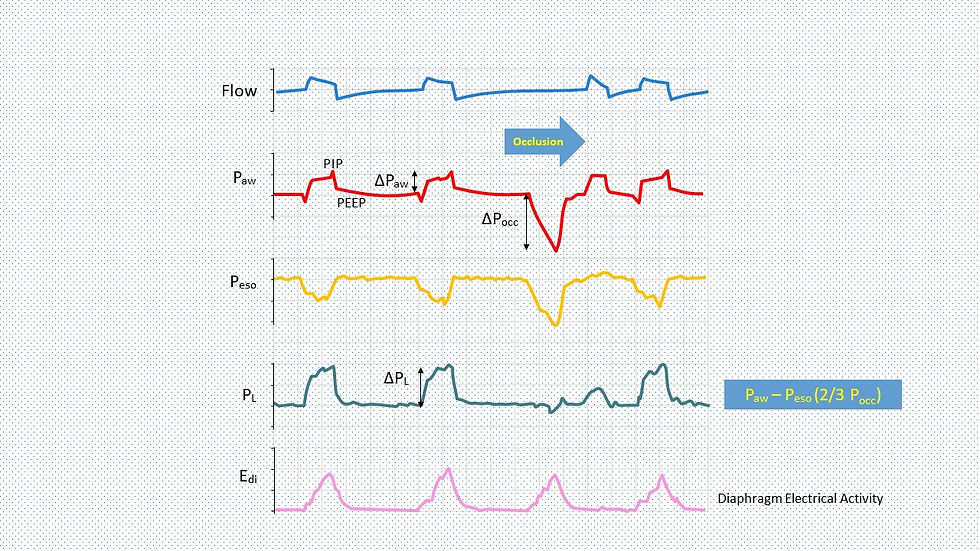
Mechanical ventilation may have both beneficial and deleterious effects depending on the patient's inspiratory effort. Inspiratory effort increases tidal volume and global dynamic lung stress in pressure-targeted modes of ventilation, potentially leading to lung injury. Vigorous inspiratory efforts can generate pendelluft and amplify regional lung stress and strain, causing regional lung injury even in volume-cycled modes of ventilation. During a randomly applied end-expiratory airway occlusion on the ventilator, the airway pressure deflection generated by the patient's respiratory effort against the occluded airway (ΔPocc) is correlated with the pressure generated by the respiratory muscles to expand the lungs and chest wall during mechanically assisted breaths. This non-invasive maneuver provides the intensivist with a very good tool to estimate the respiratory muscle pressure and transpulmonary pressure at the bedside.
In this post, we will explain the end-expiratory occlusion test and how to use it to detect excessive (potentially injurious) inspiratory effort and dynamic lung stress. We will also briefly discuss the available literature to determine its reliability in clinical practice.
Do you use End-expiratory occlusion test to predict inspiratory muscle pressure and transpulmonary pressure?
Yes
No
Never heard of it!
What is the end-expiratory occlusion test?
The test is done in mechanically ventilated patients to determine the pressure generated by the inspiratory effort of the patient against occluded airways in expiration. The maneuver entails the application of a one-way end-expiratory occlusion (similar to how we check for auto-PEEP) for 15-20 minutes permitting expiratory flow but not inspiratory flow. The operator observes the inspiratory efforts of the patient which generate negative deflections in the airway pressure. The maximal deflection in Paw from PEEP during each occlusion was recorded as a measurement of occlusion pressure (ΔPocc).
What are the benefits and use of the end-expiratory occlusion test?
The end-expiratory occlusion test provides a non-invasive means of detecting excessive inspiratory efforts and dynamic lung stress. There is a correlation between the occluded pressure and both the pressure generated by the respiratory muscles and the transpulmonary pressure. Bertoni et al. were able to predict the inspiratory muscle pressure (Pmus) at 3/4 of the change in the occlusion pressure (∆Pocc: PEEP-Pocc). The change in transpulmonary pressure (ΔPL) equaled the change in airway pressure (Paw) plus the change in esophageal pressure estimated at 2/3 of the occlusion pressure [1].
The predicted Pmus helps in determining the extent of respiratory muscle excitation and work, hence, the clinician will be able to adjust mechanical ventilation settings and sedation to target pmus ≥ 3 to 5 cm H2O to avoid over-assistance myotrauma and ≤ 10 to 15 cm H2O to avoid under-assistance myotrauma. On the other hand, the predicted ΔPL should be minimized to ≤ 15-17 cm H2O minimizing the dynamic lung stress and avoiding volutrauma and barotrauma.
How reliable is the test?
In the same study by Bertoni et al, the ΔPocc measurements accurately detected Pmus > 10 cm H2O (area under the receiver operating curve (AUROC) 0.92, 95% CI 0.83–0.97) and ΔPL,dyn > 15 cm H2O (AUROC 0.93, 95% CI 0.86–0.99). This study is rather small with a total of in 16 patients with fifty-two daily recordings.
In another study in COVID-19 patients (known to have a high respiratory drive), excessive ∆PL > 20 cmH2O and Pmus > 15 cmH2O were accurately detected (AUROC 1.00 [95% CI, 1.00–1.00]) with high sensitivity and specificity. The study included a total of 13 patients [2].
In the above two studies, the authors commented that "computed ∆PL and Pmus cannot replace ∆PL and Pmus derived from esophageal manometry, but they can predict excessive ∆PL and Pmus with high accuracy".
Conclusion
The end-expiratory occlusion test is a non-invasive way of detecting excessive inspiratory efforts and dynamic lung stress. The test has been shown to be reliable in predicting the pressure generated by the respiratory muscles and transpulmonary pressure. This information can help the clinician in adjusting mechanical ventilation and sedation settings.
REFERENCES
Bertoni, M., Telias, I., Urner, M. et al. A novel non-invasive method to detect excessively high respiratory effort and dynamic transpulmonary driving pressure during mechanical ventilation. Crit Care 23, 346 (2019). https://doi.org/10.1186/s13054-019-2617-0.
Roesthuis, L., van den Berg, M. & van der Hoeven, H. Non-invasive method to detect high respiratory effort and transpulmonary driving pressures in COVID-19 patients during mechanical ventilation. Ann. Intensive Care 11, 26 (2021). https://doi.org/10.1186/s13613-021-00821-9





Kaiser OTC benefits provide members with discounts on over-the-counter medications, vitamins, and health essentials, promoting better health management and cost-effective wellness solutions.
Obituaries near me help you find recent death notices, providing information about funeral services, memorials, and tributes for loved ones in your area.
is traveluro legit? Many users have had mixed experiences with the platform, so it's important to read reviews and verify deals before booking.
Thanks fir the easy and valuable explanation
of course you mean 15-20 sec not min, right?