
Airway Clearance in Mechanically Ventilated Patients
Cough is a vital method of eliminating mucus from the upper and lower airways. Mechanical ventilation in the intensive care setting impedes coughing and clearance of the airway as it prevents the patients from closing the glottis and it reduces the cough's power to drive secretions away. Furthermore, severely ill patients frequently have a weak or no cough reflex due to altered levels of consciousness, sedation, muscular weakness, or muscle paralysis. As a result, severely ill patients being subjected to invasive ventilation are susceptible to sputum retention, sputum accumulation, atelectasis, and ventilator-associated pneumonia [1].
With a defective cough mechanism, the patient is dependent on mucociliary clearance to clear airways which is not a very effective way. Therefore, the aspiration of secretions through repeated endotracheal suctioning becomes a core measure in ventilated patients. Nevertheless, the effectiveness of endotracheal suctioning is limited as it is confined to a small portion of the airway. Sputum retention, resulting from an inability to cough efficiently, is one risk factor for extubation failure and is linked to increased morbidity and mortality. In addition, invasive suction is linked to complications such as hypoxia, tissue damage, and infection [2].
Cough Assist Devices
Cough assist devices are positive pressure ventilation machines that can help a person cough up secretions and improve the clearance of the airway. There are many different types of cough assist devices, but they all work based on the same mechanism. In awake patients, the device applies positive pressure to the airway and then abruptly releases the pressure. This change in pressure creates a “cough flow” that can help to move secretions from the lungs.
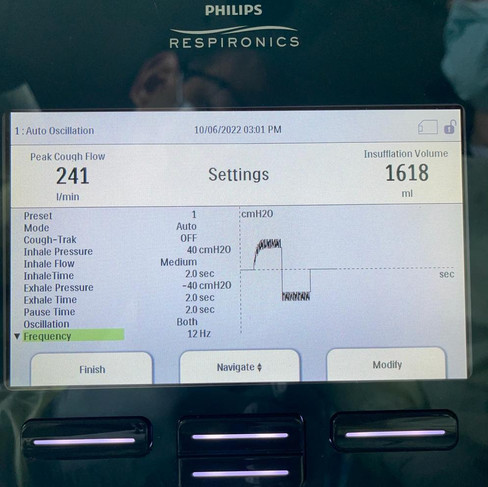
In mechanically ventilated patients cough assistance is performed through the application of rapidly alternating positive and negative pressures, which approximates a normal cough. Mechanical insufflation-exsufflation protocols generally consist of 3–5 cycles of positive pressure ranging from + 15 cm H2O to a maximum pressure of + 40 cm (insufflation), followed by a negative pressure ranging from − 15 cm H2O to a maximum of − 40 cm H2O (exsufflation). This technique augments inspiratory and expiratory flows to improve sputum mobilization. Oscillation is utilized at a different Hz frequency on either phase of the procedures or both to enhance the mobilization of secretions. The operator can determine the length of each phase and a pause may be appended after that. Tracheal suctioning is usually done after the treatment.
What does the evidence say?
Mechanical insufflation-exsufflation aids sputum clearance from the upper and lower airways and improves airway clearance. The available evidence for cough assist devices in the intensive care unit is very limited. Most of the evidence is in patients with neuromuscular diseases where mechanical insufflation/exsufflation augments the patient's cough. One study shows that the cough assist device produces a greater increase in peak cough flow than other standard cough augmentation techniques in adults and children with neuromuscular disease [3]. Another study shows that cough-assist therapy reduces recurrent respiratory infections in patients with the neuromuscular disease [4]. In patients on mechanical ventilation, mechanical insufflation-exsufflation through a tracheostomy tube with an inflated cuff was more successful at removing airway secretions in ventilator-dependent persons with amyotrophic lateral sclerosis than conventional tracheal suctioning, according to a small pilot study [5]. On the other hand, a study published in the Indian Journal of Critical Care Medicine in 2018 revealed that mechanical insufflation–exsufflation does not enhance airway clearance in mechanically ventilated individuals [6].
Conclusion
Mechanical insufflation-exsufflation is a technique that uses pressure to help clear secretions from the lungs. There is limited evidence on the effectiveness of this technique in mechanically ventilated patients, but some studies have shown that it can be helpful in patients with neuromuscular diseases.
REFERENCES
References
AARC Clinical Practice Guideline: Effectiveness of Non Pharmacologic Airway Clearance Therapies in Hospitalized Patients, Respiratory Care Journal, Dec 2013, Vol 58 N°12
AARC Clinical Practice Guideline. Endotracheal suctioning of mechanically ventilated adults and children with artificial airways. Respiratory Care 1993;38(5)500-504.
Chatwin M, Ross E, Hart N, Nickol AH, Polkey MI, Simmonds AK. Cough Augmentation with Mechanical Insufflation/Exsufflation in Patients with Neuromuscular Weakness. Eur Respir J: March 2003; 21(3):502-508.
Alice C. Tzeng and John R. Bach. Prevention of Pulmonary Morbidity in Patients with Neuromuscular Disease. Chest 2000;118:1390-1396. DOI 10. 1378/Chest 118.5.1390.
Sancho J, Servera E, Vergara P, Marín J. Mechanical insufflation-exsufflation vs. tracheal suctioning via tracheostomy tubes for patients with amyotrophic lateral sclerosis: a pilot study. Am J Phys Med Rehabil. 2003 Oct;82(10):750-3.
Coutinho WM, Vieira PJC, Kutchak FM, Dias AS, Rieder MM, Forgiarini LA Jr. Comparison of Mechanical Insufflation-Exsufflation and Endotracheal Suctioning in Mechanically Ventilated Patients: Effects on Respiratory Mechanics, Hemodynamics, and Volume of Secretions. Indian J Crit Care Med. 2018 Jul;22(7):485-490.





Kaiser OTC benefits provide members with discounts on over-the-counter medications, vitamins, and health essentials, promoting better health management and cost-effective wellness solutions.
Obituaries near me help you find recent death notices, providing information about funeral services, memorials, and tributes for loved ones in your area.
is traveluro legit? Many users have had mixed experiences with the platform, so it's important to read reviews and verify deals before booking.